Hepatitis C Virus
You have been diagnosed with hepatitis C, also called HCV. Hepatitis is an inflammation of the liver. In your case, it's from an infection with the hepatitis C virus.
Causes
The most common causes of hepatitis are viruses. Alcohol and drug abuse, chemical toxins, and immune system problems can also cause hepatitis. So can diabetes, obesity, and the metabolic syndrome.
When a virus causes hepatitis, it's called viral hepatitis. The hepatitis viruses A, B, and C commonly cause viral hepatitis. Other viral infections can also cause hepatitis, such as the viruses that cause mononucleosis and chickenpox.
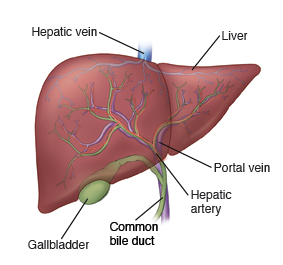
What all the liver (hepatic) viruses have in common is that once they are spread to you, they infect the liver and then cause inflammation (hepatitis). The different viruses are spread in different ways. But many of them can affect your health over a long time. Possible complications include cirrhosis, liver cancer, and liver failure. Hepatitis A does not cause long-term (chronic) liver disease.
HCV is commonly spread through injection of contaminated body fluids or blood products, transfusions, or IV (intravenous) drug use. It can also be spread through tattoos or piercing with nonsterile tools, or certain medical procedures. The risk of getting hepatitis C from someone you are close to and from sexual contact is very low.
There is currently no vaccine for HCV. Staying away from the common causes is the best way to stay away from infection.
Symptoms
Many people with hepatitis C have no symptoms or only mild ones when they are first infected. Often this is also the case for many years later. But HCV can damage your liver. And for people infected in adulthood, it usually becomes chronic (long-term) without treatment. Symptoms in the early stages can include:
-
Tiredness, fatigue, or weakness
-
Low-grade fever
-
Loss of appetite
-
Upset stomach, diarrhea, nausea, or vomiting
-
Belly (abdominal) pain
-
Dark yellow urine
-
Light-colored or pale stool (gray or clay color)
-
Yellow color of the skin or eyes (jaundice)
-
Joint pain
These symptoms can be caused by many different conditions. Because these symptoms are not specific to HCV, many people are not diagnosed for a long time. HCV can become chronic in more than 50% of people who are infected as adults. Infants infected at birth by infected mothers are more likely to spontaneously clear the infection. Chronic HCV infection means that you carry the virus and can spread the disease to others. Most people with chronic infection (about 70%) will develop some degree of chronic liver disease. For many, this may cause no symptoms or long-term effects. But over time there is a 20% chance of having healthy liver tissue replaced by scar tissue (cirrhosis). Heavy alcohol drinkers and people with chronic hepatitis B infection are at greatest risk for long-term problems. So are people whose livers are also inflamed from fatty liver disease (a condition called metabolic dysfunction-associated steatohepatitis).
Anyone who has chronic hepatitis C should be treated with medicines to cure the infection. Since 2014 safe and effective treatment against hepatitis C became available. Over 95% of people are cured with a 8 to 12-week course of oral medicine. There is currently no vaccine to protect against hepatitis C infection. If you have cirrhosis at the time of cure, there is a chance that your liver may even heal to some degree. If you have cirrhosis, you will need to follow closely with your doctor to watch for health risks associated with cirrhosis, such as hepatomas (liver cancer), ascites (fluid in the belly), and esophageal varices (dilated veins in the esophagus that can bleed).
Home care
-
A diet low in saturated fats and high in fruits and vegetables is best for you and your liver. Have small, frequent meals if you experience nausea.
-
If you are having symptoms of hepatitis, you may fatigue easily. Get lots of rest. Don't exert yourself too much.
-
Acetaminophen and nonsteroidal anti-inflammatory drugs, such as ibuprofen and naproxen, can be toxic to the liver in high doses with prolonged use, or if there is existing liver damage.
-
If you have hepatitis, don't take these medicines until you talk about them with your doctor.
-
If you have only mild or no liver damage from chronic hepatitis, you may take acetaminophen in low doses (2 grams per 24 hours) if approved by your doctor. Don't take anti-inflammatory medicines. Never take acetaminophen with alcohol since this increases the risk of liver damage.
-
Alcohol stresses the liver. People with hepatitis shouldn't drink alcohol. It can make the disease worse.
Preventing the spread of hepatitis
-
HCV is most often spread by blood contact. Never share needles, syringes, tattoo equipment, or snorting straws.
-
Don't try to donate blood, organs, tissues, or semen.
-
Don't share razors or toothbrushes, although it's very rare to pass along hepatitis C this way.
-
If you need medical or dental care, tell the staff that you have hepatitis.
-
If you're pregnant or plan to be pregnant, tell your doctor. There is a small chance that hepatitis C can be passed along to the unborn baby. HCV isn't passed in breastmilk.
-
The risk of spreading the virus through sex is low, especially if you only have sex with 1 partner. Standard safer-sex practices, including using latex condoms, are advised if you have sex with more than 1 partner. There is no need to change your sexual practices if you are in a long-term relationship with 1 partner.
-
The risk of household spread is low. There is no need to stay away from close contact or not share meals or utensils.
-
HCV does not involve any restrictions on work.
Follow-up care
Follow up with your doctor, or as advised. Ask about hepatitis A and B vaccines. You are at greater risk of getting these types of the disease, and they could cause more damage to your liver. Your sexual partner should contact their doctor and have a test to see if they have been infected with HCV.
If X-rays, a CT scan, an MRI, or an ultrasound was done, they will be reviewed by a specialist. You will be given the results, especially if they affect your treatment.
Call 911
Call 911 if any of the following occur:
-
Trouble breathing or swallowing, wheezing
-
Confusion
-
Extreme drowsiness or trouble waking up
-
Fainting or loss of consciousness
-
Fast heart rate
-
Vomiting blood or significant rectal bleeding (red blood or black, tarry stool)
When to get medical advice
Call your doctor or get medical care right away if any of the following occur:
-
Frequent vomiting
-
Weight loss from poor appetite
-
Increase in belly pain or swelling
-
Increasing drowsiness or confusion
-
Weakness or dizziness
-
New or increasing yellow color of skin or eyes (jaundice)
-
Bleeding from the gums or nose, or easy bruising