Head Injury with Sleep Monitoring (Child)
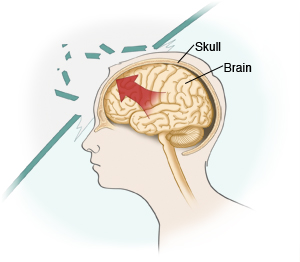
Your child has a head injury. It doesn't look serious at this time. But symptoms of a more serious problem may appear later. This includes mild brain injury (concussion) or bruising or bleeding in the brain. For this reason, you'll need to watch your child for the symptoms listed below. Once at home, also be sure to follow any care instructions you’re given for your child.
Home care
Watch for the following symptoms
For the next 24 hours (or longer, if directed), you or another adult must stay with your child. If your child is resting, they will need to be woken up every 2 hours, or as advised, to be checked for symptoms. This is called sleep monitoring. Symptoms to watch for include:
-
Headache
-
Nausea or vomiting
-
Dizziness
-
Sensitivity to light or noise
-
Unusual sleepiness or grogginess
-
Trouble falling asleep
-
Personality changes
-
Vision changes
-
Memory loss
-
Confusion
-
Trouble walking or clumsiness
-
Loss of consciousness (even for a short time)
-
Inability to be awakened
-
Stiff neck
-
Weakness or numbness in any part of the body
-
Seizures
For young children, also watch for crying that can’t be soothed or refusal to feed. Also check for any signs of changes to the head, such as bruising, bulging, or a soft or pushed-in spot.
If your child develops any of these symptoms, get emergency medical care right away. If none of these symptoms are noted during the first 24 hours, keep watching for symptoms for the next day or so. Ask the provider if sleep monitoring needs to be continued during this time.
General care
-
If your child was prescribed medicines for pain, give them to your child as directed. Don’t give your child other pain medicines without checking with the provider first.
-
To help reduce swelling and pain, apply a cold source to the injured area for up to 20 minutes at a time. Do this as often as directed. Use a cold pack or bag of ice wrapped in a thin towel. Never apply a cold source directly to the skin.
-
If your child has cuts or scrapes on the face or scalp, care for them as directed.
-
For the next 24 hours (or longer, if advised), your child should:
-
Not lift or do other strenuous activities
-
Not play sports or any other activities that could result in another head injury
-
Limit TV, smartphones, video games, computers, and music—or avoid them completely. These activities may make symptoms worse.
Follow-up care
Follow up with your child’s healthcare provider as directed. If imaging tests were done, they will be reviewed by a healthcare provider. You will be told the results and any new findings that may affect your child’s care.
When to get medical advice
Unless told otherwise, call your child's healthcare provider right away if any of these occur:
-
Pain that doesn’t get better or worsens
-
New or increased swelling or bruising
-
Increased redness, warmth, drainage, or bleeding from the injured area
-
Fluid drainage or bleeding from the nose or ears
-
Sick appearance or behaviors that worry you
-
Lethargy or excessive sleepiness
-
Bruising behind the ears or around the eyes
-
Worsening headache
-
Vomiting that worsens
-
Double vision
-
Trouble walking or talking
Fever and children
Use a digital thermometer to check your child’s temperature. Don’t use a mercury thermometer. There are different kinds and uses of digital thermometers. They include:
-
Rectal. For children younger than 3 years, a rectal temperature is the most accurate.
-
Forehead (temporal). This works for children age 3 months and older. If a child under 3 months old has signs of illness, this can be used for a first pass. The provider may want to confirm with a rectal temperature.
-
Ear (tympanic). Ear temperatures are accurate after 6 months of age, but not before.
-
Armpit (axillary). This is the least reliable but may be used for a first pass to check a child of any age with signs of illness. The provider may want to confirm with a rectal temperature.
-
Mouth (oral). Don’t use a thermometer in your child’s mouth until they are at least 4 years old.
Use the rectal thermometer with care. Follow the product maker’s directions for correct use. Insert it gently. Label it and make sure it’s not used in the mouth. It may pass on germs from the stool. If you don’t feel OK using a rectal thermometer, ask the healthcare provider what type to use instead. When you talk with any healthcare provider about your child’s fever, tell them which type you used.
Below are guidelines to know if your young child has a fever. Your child’s healthcare provider may give you different numbers for your child. Follow your provider’s specific instructions.
Fever readings for a baby under 3 months old:
-
First, ask your child’s healthcare provider how you should take the temperature.
-
Rectal or forehead: 100.4°F (38°C) or higher
-
Armpit: 99°F (37.2°C) or higher
Fever readings for a child age 3 months to 36 months (3 years):
-
Rectal, forehead, or ear: 102°F (38.9°C) or higher
-
Armpit: 101°F (38.3°C) or higher
Call the healthcare provider in these cases:
-
Repeated temperature of 104°F (40°C) or higher in a child of any age
-
Fever of 100.4° (38°C) or higher in baby younger than 3 months
-
Fever that lasts more than 24 hours in a child under age 2
-
Fever that lasts for 3 days in a child age 2 or older