Heart Disease Education
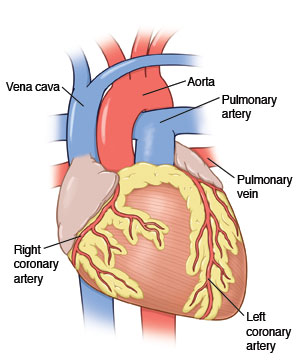
The heart beats 60 to 100 times per minute, 24 hours a day. This equals almost 100,000 times a day. It pumps blood with oxygen and nutrients to the tissues and organs of the body. But the heart is a muscle and needs its own supply of blood. Blood flow to the heart is supplied by the coronary arteries. Coronary artery disease (atherosclerosis) is a result of cholesterol, saturated fat, and calcium deposits (plaques) that build up inside the walls. This causes inflammation within the coronary arteries. These plaques narrow the artery and reduce blood flow to the heart muscle. The reduction in blood flow to the heart muscle decreases oxygen supply to the heart. If the narrowing is significant enough, the oxygen supply to one or more regions of the heart can be temporarily or permanently shut down. Sometimes the plaque can burst open (rupture), exposing the materials in the plaque to the bloodstream. This can lead to a blood clot suddenly forming on top of the plaque, which interrupts blood flow to the heart muscle. This can cause chest pain (angina) and possibly death of heart tissue (heart attack).
Types of chest pain
Angina is the name for pain in the heart muscle. Angina is a warning sign of serious heart disease. When untreated, it can lead to a heart attack, also known as acute myocardial infarction, or AMI. Angina occurs when there isn't enough blood and oxygen flowing to the heart for the amount of work it is doing. This most often happens during physical exertion, when the heart is working hardest. It is usually relieved by rest or nitroglycerin. Angina may also occur after a large meal, when extra blood is sent to the digestive organs and less goes to the heart. In the case of advanced or unstable heart disease, angina can occur at rest or can wake you up from sleep. Angina usually lasts from a few minutes up to 20 minutes or more. When treated early, the effects of angina can be reversed without permanent damage to the heart. Angina is a serious condition and needs to be checked by a health care provider right away.
There are two types of angina—stable and unstable:
-
Stable angina. This often occurs with a predictable level of activity. Being stable, its character, severity, and occurrence don't change much over time. It often starts with activity and resolves with rest or taking your medicine as instructed by your health care provider. The symptoms usually don't last long.
-
Unstable angina. This changes or gets worse over time. It is different from whatever you are used to. It may feel different or worse, begin without cause, occur with exercise or exertion, wake you up from sleep, and last longer. It may not respond in the same way as it does when you take your usual medicines for an attack. This type of angina can be a warning sign of an impending heart attack.
A heart attack is often the result of a blood clot that suddenly forms in a coronary artery that has been narrowed with plaque. When this occurs, blood flow may be cut off to a part of the heart muscle, causing the cells to die. This weakens the pumping action of the heart, which affects the delivery of blood to all the other organs in the body, including the brain. If not treated right away, this damage will become permanent. The earlier that treatment is given, the better chance that the heart muscle can be saved.
The pain you feel with angina and a heart attack may have a similar quality. But it's is usually different in intensity and duration. Here are some typical descriptions of a heart attack:
-
It's most often felt as a squeezing, crushing, pressure-like sensation in the center of the chest.
-
It's sometimes described as “something heavy sitting on my chest.”
-
It may feel more like a bad case of indigestion.
-
The pain may spread from the chest to the arm, shoulder, throat, or jaw.
-
Sometimes the pain isn't felt in the chest at all, but only in the arm, shoulder, throat, or jaw.
-
There may also be nausea, vomiting, dizziness or lightheadedness, sweating, and trouble breathing.
-
It may cause unexplained weakness.
You may not be able to tell the difference between "bad" angina and a heart attack at home. Get help if your symptoms are different than usual. Don't be in denial or just try to tough it out.
Call 911
It's important to call 911. This is the fastest and safest way to get to the ER. Don't delay. You may be having a heart attack. The paramedics can also start treatment on the way to the hospital. This saves valuable time for your heart.
Call 911 right away if:
Other reasons to call 911
Don't wait until symptoms become severe to call 911. Other reasons to call 911 include:
-
Trouble breathing.
-
Feeling lightheaded, faint, or dizzy.
-
A rapid heartbeat.
-
A heart rate that's slower than usual.
-
Angina with weakness, dizziness, fainting, heavy sweating, nausea, or vomiting.
-
Extreme drowsiness or confusion.
-
Weakness of an arm or leg or one side of the face.
-
Trouble with speech or vision.
After you call 911
After you call 911:
-
Take a second nitroglycerin tablet or spray unless instructed otherwise. When repeating doses, sit down, if possible, because it can make you feel lightheaded or dizzy.
-
Wait another 5 minutes. If the angina still doesn't go away, take a third nitroglycerin tablet or spray. Don't take more than 3 tablets or sprays within 15 minutes.
-
Stay on the phone with 911 for more instructions.
Note: Your health care provider may give you slightly different instructions than those above. If so, follow them carefully.
When to get medical care
Remember, the signs and symptoms of a heart attack aren't always like they are on TV. Sometimes they aren't so obvious. You may only feel weak or just not right. If it isn't clear or if you have any doubt, call for advice.
-
Get help if there's a change in the type of pain, if it feels different, or if your symptoms are mild.
-
Don't drive yourself. Have someone else drive you. If no one can drive, call 911.
-
Don't delay. Fast diagnosis and treatment can prevent or limit the amount of heart damage during a heart attack.
-
Don't go to your health care provider's office or a clinic. They may not be able to provide all the testing and treatment needed for this condition.
-
If your provider has given you medicines to take when symptoms occur, take them. But don't delay getting help by trying to locate medicines.
What happens in the emergency room (ER)
The emergency room (ER) is connected to your local emergency medical system (EMS) through 911. That's why during a cardiac emergency, calling 911 is the fastest way to get help. The goal of the ER is to quickly screen, evaluate, and treat people.
When you're there, an electrocardiogram (ECG) will be done. Often this will be done by paramedics who will send it to the hospital even before you get to the ER. Blood samples may be taken. These look for the presence of heart enzymes that leak from damaged heart cells and show if a heart attack is occurring. You'll often be evaluated by a heart specialist (cardiologist) who decides the best course of action. In the case of severe angina or early heart attack, and depending on the circumstances, powerful clot-busting medicines can be used to dissolve blood clots in the coronary artery.
In most cases, you may be taken to a cardiac catheterization lab for emergency angiography and coronary intervention. During this procedure, a long, thin, plastic tube (catheter) is put in an artery in your groin or arm. It's threaded through the blood vessel to the blockage. Blood flow will be evaluated. If a significant blockage is seen, a balloon and metal mesh coil (stent) may be inserted. This is done to open the artery and restore blood flow.
Risk factors for heart disease
Some risk factors for heart disease are things you can change. Others can't be changed, such as your family history. Many risk factors work by either directly or indirectly damaging the blood vessels of the heart, or by increasing the risk of forming blood or cholesterol clots. These then clog up and block the arteries.
Physical lifestyle risk factors include:
-
Cigarette smoking or tobacco use.
-
High blood pressure.
-
High blood cholesterol.
-
Use of stimulant drugs, such as cocaine, crack, and methamphetamine.
-
Eating high-fat, high-cholesterol foods.
-
Diabetes.
-
Overweight and obesity, which increases the risk for diabetes and high blood pressure.
-
Lack of regular physical activity.
-
Lack of sleep.
Emotional lifestyle factors include:
-
Chronic high stress levels, which release stress hormones. These raise blood pressure and cholesterol levels and make blood clot more easily.
-
Held-in anger and a hostile or cynical attitude.
-
Social and emotional isolation and lack of intimacy.
-
Loss of a relationship.
-
Depression.
Other factors that increase the risk of heart attack are things you can't control. These include:
-
Age. The older you get beyond 40, the greater your risk is of significant coronary artery disease.
-
Being male. More men than women get heart disease. (But after menopause, a woman's risk of heart disease dramatically increases.)
-
Family history. If your mother, father, brother, or sister has coronary artery disease, your risk of having it is higher than a person your age without this family history.
What you can do to decrease your risk
To reduce your risk for heart disease:
-
Get regular checkups with your health care provider.
-
Take your medicines for blood pressure, cholesterol, or diabetes as directed.
-
Watch your diet. Eat a heart-healthy diet, choosing fresh foods, less salt, cholesterol, and fat.
-
Stop smoking. Get help if needed.
-
Stop using illegal drugs.
-
Get regular exercise.
-
Manage stress.
-
Get enough sleep.
-
Ask your provider if they recommend behavioral counseling to promote a healthy diet and physical activity.