Heat Rash (Child)
Heat rash is a skin irritation that happens when sweat gets trapped in the skin. It’s also known as prickly heat. The rash shows up as little red bumps and sometimes tiny blisters on the skin. The rash may itch. It's common in young children.
Normally, sweat glands help the body stay cool by releasing the salty fluid called sweat. But sweat glands don’t become fully active until puberty. Because of this, sweat can get trapped in the skin more easily in young children.
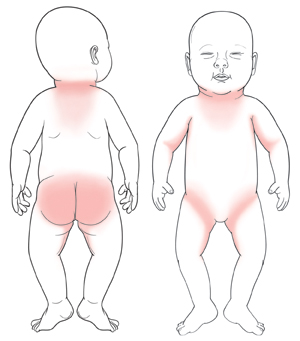
In babies, heat rash is mainly found on the head, neck, shoulders, chest, and back. It can also occur in the armpits and groin. Older children tend to get heat rash on their neck, upper chest, groin, and under wrist folds.
Heat rash happens most often in hot and humid weather, or when a child is dressed too warmly. Heat rash often goes away on its own and doesn’t need medical care. The best way to relieve symptoms is to cool the skin.
Home care
Try these tips when caring for your child at home:
-
Bathe your child in lukewarm water and use mild soap. After bathing, let the skin air dry. You can also place a washcloth dipped in cool water on the rash area.
-
Don’t use ointments on your child’s skin. These don’t improve or prevent heat rash. Ointment tends to keep the skin warmer and block the pores. Don't use talcum powder. It's harmful to the lungs and genital area.
-
Try to prevent your child from scratching the rash. Scratching can delay healing. It may also cause an infection.
-
Keep your child cool and dry during warm weather. Use air conditioning or a fan. Dress your child in lightweight, soft cotton clothing.
Follow-up care
Follow up with your child’s health care provider, or as advised.
When to get medical advice
Call your child's health care provider right away if any of these occur:
-
Fever
-
Changes in the rash color to dark purple
-
Rash spreads
-
Swollen lymph nodes in the armpit, neck, or groin
-
New symptoms, such as redness, swelling, or pain
-
Bad-smelling fluid coming from the rash
Fever and children
Use a digital thermometer to check your child’s temperature. Don’t use a mercury thermometer. There are different kinds and uses of digital thermometers. They include:
-
Rectal. For children younger than 3 years old, a rectal temperature is the most accurate.
-
Forehead (temporal). This works for children age 3 months and older. If a child under 3 months old has signs of illness, this can be used for a first pass. The provider may want to confirm with a rectal temperature.
-
Ear (tympanic). Ear temperatures are accurate after 6 months of age, but not before.
-
Armpit (axillary). This is the least reliable but may be used for a first pass to check a child of any age with signs of illness. The provider may want to confirm with a rectal temperature.
-
Mouth (oral). Don’t use a thermometer in your child’s mouth until they are at least 4 years old.
Use the rectal thermometer with care. Follow the product maker’s directions for correct use. Insert it gently. Label it and make sure it’s not used in the mouth. It may pass on germs from the stool. If you don’t feel OK using a rectal thermometer, ask the health care provider what type to use instead. When you talk with any health care provider about your child’s fever, tell them which type you used.
Below are guidelines to know if your young child has a fever. Your child’s health care provider may give you different numbers for your child. Follow your provider’s specific instructions.
Fever readings for a baby under 3 months old:
-
First, ask your child’s health care provider how you should take the temperature.
-
Rectal or forehead: 100.4°F (38°C) or higher
-
Armpit: 99°F (37.2°C) or higher
Fever readings for a child age 3 months to 36 months (3 years):
-
Rectal, forehead, or ear: 102°F (38.9°C) or higher
-
Armpit: 101°F (38.3°C) or higher
Call the health care provider in these cases:
-
Repeated temperature of 104°F (40°C) or higher in a child of any age
-
Fever of 100.4° (38°C) or higher in baby younger than 3 months
-
Fever that lasts more than 24 hours in a child under age 2
-
Fever that lasts for 3 days in a child age 2 or older