Urinary Incontinence (Male)
We understand that gender is a spectrum. We may use gendered terms to talk about anatomy and health risk. Please use this sheet in a way that works best for you and your doctor as you talk about your care.
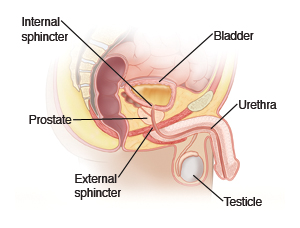
Urinary incontinence means not being able to control the release of urine from the bladder.
Causes
Common causes of urinary incontinence in men include:
-
Infection.
-
Certain medicines.
-
Aging.
-
Poor pelvic muscle tone.
-
Bladder spasms.
-
Obesity.
-
Enlarged prostate.
-
Prostatitis, a painful inflammation of the prostate gland.
-
Trouble urinating and fully emptying the bladder (urinary retention).
Other things that can cause incontinence are:
-
Nervous system diseases, such as multiple sclerosis, Parkinson’s disease, and spinal cord injuries.
-
Diabetes.
-
Sleep apnea.
-
Urinary tract infections.
-
Prostate surgery.
-
Pelvic injury.
-
Tumors and kidney stones.
Constipation and smoking have also been identified as risk factors.
Types of incontinence
-
Urge incontinence (overactive bladder). This is a sudden urge to urinate. It occurs even though there may not be much urine in the bladder. The need to urinate often during the night is common. It's due to overactive bladder muscles. Sometimes it can be a sign of a urinary tract infection.
-
Stress incontinence. This is urine leakage that you can't control. It can occur whenever the pressure increases in your abdomen (belly). This includes sneezing, coughing, lifting heavy objects, exercising, and other actions that put stress on the bladder.
-
Overflow incontinence. This happens when your bladder doesn't empty all the way and too much urine is left in your bladder. As your bladder gets too full, the urine starts leaking. It can happen if your prostate is enlarged and is blocking the flow of urine. Spinal cord injuries, multiple sclerosis, or diabetes can also affect the bladder muscle function. Other causes can include pelvic masses and pelvic organ prolapse.
-
Functional incontinence. This happens when the urine loss is from thinking or physical problems, such as physical or mental disability, trouble speaking, or other problems communicating your need to go to the toilet. It is sometimes referred to as toileting difficulty. For example, a person with Alzheimer's disease may not realize they need to plan to use the toilet.
-
Mixed incontinence. This is usually a combination of stress and urge incontinence.
-
Transient incontinence. This happens due to a temporary situation, such as an infection or new medicine. Once the cause is removed, the incontinence goes away.
Treatment
Treatment depends on what is causing the condition. Bladder infections are treated with antibiotics. Urinary retention may be treated with a bladder catheter until the underlying cause can be treated.
Home care
Follow these guidelines when caring for yourself at home:
-
Avoid foods and drinks that may irritate the bladder. These include:
-
Limit fluids to 6 to 8 cups a day unless your doctor gives other instructions.
-
Lose weight if you are overweight. This may reduce your symptoms.
-
If advised, do regular pelvic muscle-strengthening exercises, such as Kegel exercises.
-
Keep a bladder or voiding diary. This would include the amount of fluids you drink and when you drink them, It would also include the time of any urine leakage, and how often you urinate.
-
Train your bladder. This means urinating according to a schedule. Based on information from your bladder diary, your doctor can help you make a schedule. Once you have adjusted to it, you can wait a little longer between your trips to the toilet. Your bladder will gradually regain its strength to hold the urine longer.
-
If needed, wear absorbent pads to catch urine. Change the pads often. This is for good hygiene and to prevent skin and bladder infections.
-
Bathe daily for good hygiene.
-
If your doctor prescribed antibiotics, take them as directed. Do not stop taking them just because you feel better. You need to take the full course of antibiotics.
-
If a catheter was left in place, keep bacteria from getting into the collection bag. Don't disconnect the catheter from the collection bag. Use a leg band to secure the catheter drainage tube, so it doesn't pull on the catheter. Drain the collection bag when it becomes full. To do this, use the drain spout at the bottom of the bag. Don't disconnect the bag from the catheter. Don't pull on or try to remove a catheter. It must be removed by a doctor.
-
If you smoke, quit. Ask your doctor if you need help.
-
If you have diabetes, keep your blood sugar under control.
-
Keep your bowel movements regular to prevent constipation. Try increasing the fiber in your diet.
-
Keep hallways clear and the bathroom clutter-free, with a light on at all times.
-
If you can't get to a regular toilet in time, use portable devices. These include commode seats or bedside commodes, bedpans, and urinals.
Follow-up care
Follow up with your doctor, or as advised.
When to contact your doctor
Contact your doctor right away if:
-
You have a fever over 100.4ºF (38°C), or as directed by your doctor.
-
You have pain or fullness in your bladder.
-
You have belly swelling, nausea, or vomiting.
-
You have back pain.
-
You have weakness, dizziness, or fainting.
-
If a catheter was left in place, and:
-
You have pain or burning when you urinate.
-
You have trouble starting your urine flow.
Online Medical Reviewer:
Melinda Murray Ratini DO
Online Medical Reviewer:
Raymond Kent Turley BSN MSN RN
Online Medical Reviewer:
Vinita Wadhawan Researcher
Date Last Reviewed:
5/1/2025
© 2000-2025 The StayWell Company, LLC. All rights reserved. This information is not intended as a substitute for professional medical care. Always follow your healthcare professional's instructions.